The Story Behind Genius Digital Diagnostics, the Breakthrough AI Innovation That Is Reinventing Cervical Cancer Screening
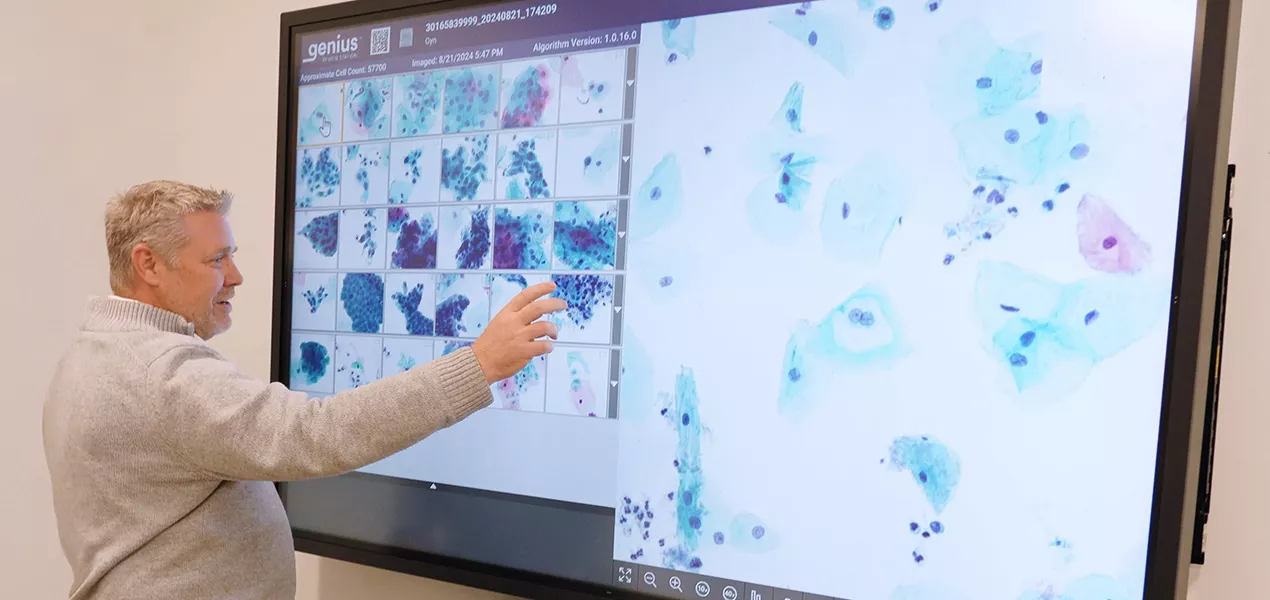
“High-grade squamous intraepithelial lesions are changes in the cells that occur before it progresses to cancer, so that's the most critical thing we can diagnose on a Pap test,” said Mike Quick. Here, he is looking at a digital case being projected onto a smartboard.*
In November 2020, the Genius™ Digital Diagnostics System arrived on the European market, unlocking new possibilities to improve laboratory workflows and more accurately detect disease. In February 2024, it became the first and only FDA-cleared AI-powered digital cytology system in the U.S. And it all began with a passionate team huddled around an empty whiteboard.
Every two minutes, a life is tragically lost to cervical cancer.1 This doesn’t have to be the case, as cervical cancer is almost entirely preventable when detected and treated early, underscoring the importance of regular screening.2 For decades checking for cervical cancer using a Pap test involved placing a patient’s sample on a slide to be examined under a microscope by a trained cytologist. But in 2014, a team at Hologic gathered around an empty whiteboard and committed to reimagining this process.
What if, instead of looking at a physical slide right in front of them, the cytologist could be located thousands of miles away, observing every cell on a computer screen? What if the technology could also use artificial intelligence (AI) to help identify pre-cancerous lesions and cervical cancer cells in a fraction of the time?
“There have been publications about the concept of digitizing cytology going back to the 1950s, but for a long time the type of imaging technology needed to do that just didn’t exist,” said Vice President of R&D, Cytology & Oncology Mike Quick, who led the team that developed what would become the Genius Digital Diagnostics System. In addition to improving disease detection and making the screening process more efficient using AI, a digitized system could allow cytologists and pathologists to review images from anywhere, potentially improving access to life-saving screenings and reducing test result turnaround times.
Finding the needle in the haystack
The first step was to develop the advanced imaging required to digitize samples. To achieve this, Quick and team developed a way to create high-magnification images from Pap test slides. Using a process called volumetric imaging, the technology takes one pass over the slide, capturing 14 focal planes — or layers — and merges them into a single layer, creating a two-dimensional representation of the slide with exceptional clarity.
“Once the high-quality image is taken, we take all that data and create a very high-resolution image from that in color because that’s what a cytologist would be used to seeing,” said Quick. “Our vision was not just to replicate the act of looking at a physical slide under a microscope, but to substantially improve the imaging experience.”
The team also needed to build an AI algorithm that could be used in a clinical setting. With tens of thousands of cells on each slide, the AI would need to be able to sift through massive amounts of data and quickly identify the needle — or needles — in a haystack to help flag abnormalities for cytologists’ review. Using thousands of existing slide images to train the AI, the team began building the complex algorithm needed for the novel technology.

Members of the Genius Digital Diagnostics team.
Quote from Mike Quick
"After we scanned that first slide and saw this sharp, in-focus image, it was a clarity we never thought possible — combined with the power of AI.”
From concept to reality
Prototype after prototype of the technology was developed, followed by extensive testing and validation. As the innovation progressed, the group of people surrounding the whiteboard and sketching out what the future of cytology could look like grew from Hologic employees to cytologists, pathologists, industry key opinion leaders and many others. Their feedback and insights into what would be the most valuable features to have in the new digital cytology system was — and continues to be — key to its success. The result? A powerful and efficient digital cytology system that allows for effective case review in a fraction of the time.
The team developed an AI algorithm that could analyze thousands of cells on each patient slide and rapidly create a gallery of the clinically relevant cells to efficiently make an interpretation. If abnormal cells are found, the high-resolution imagery can instantly be sent for review by a pathologist located anywhere across the laboratory network. “You think about all these touchpoints along the way that are now digital. Once the cytologist finishes with the case and determines it needs further review, it shows up in the pathologist’s queue almost instantly,” said Quick, noting that multiple people can view a case at the same time from different locations.
“Throughout the process there was a bit of healthy skepticism,” said Quick, who is also a trained cytologist. “I’d been in the field for 30 years and like many others, I was so used to looking through a microscope. But after we scanned that first slide and saw this sharp, in-focus image, it was a clarity we never thought possible — combined with the power of AI.”
A far-reaching impact
Since its initial launch in Europe and later launch in the U.S., more than 120 Genius Digital Diagnostics Systems are clinically in use across 16 countries. The technology continues to evolve based on feedback from healthcare providers and customers, and its potential is also being assessed for use in other disease areas.
“We’ve created a novel platform with AI and best-in-class imaging with the potential to be expanded into other cancer types and women’s health areas for an even greater impact,” said Quick. “It’s really only the beginning.”
Learn more about the Genius Digital Diagnostics System.

